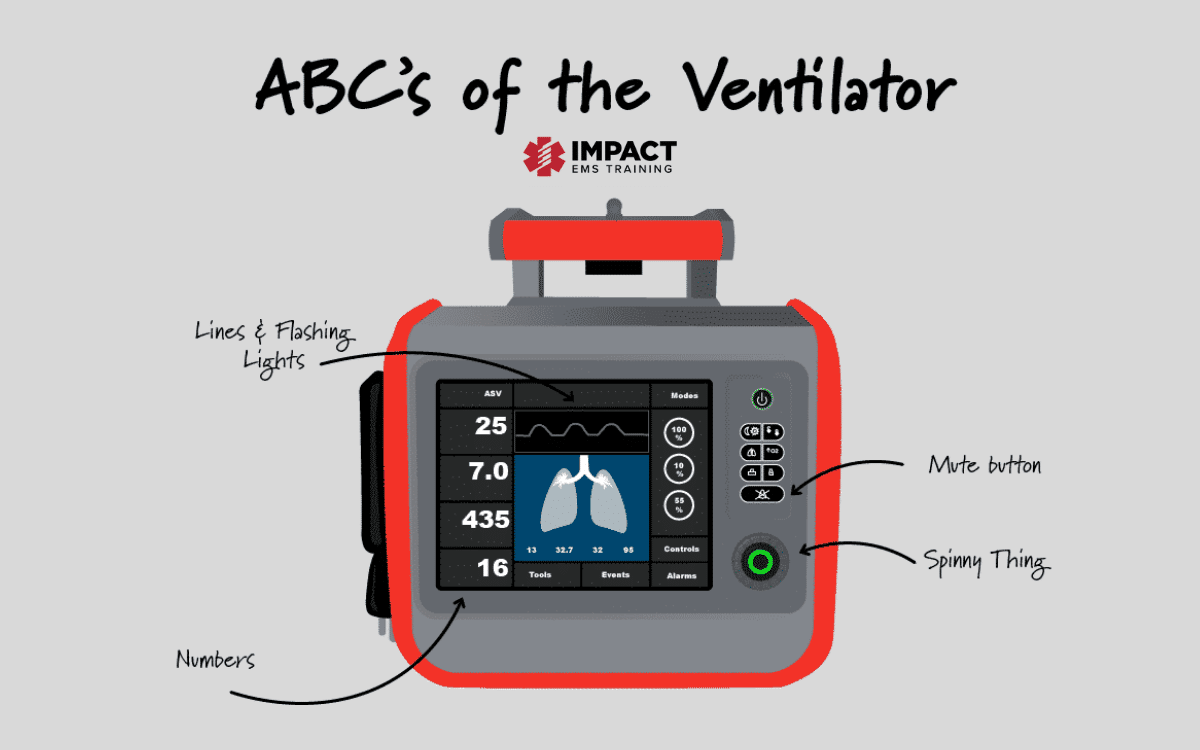
ABC’S OF THE VENTILATOR
By: Justin Krantz, NRP, CCEMT-P, FP-C
What was one of your biggest fears when starting critical care transport? Did I hear you say, “the vent?” That is ok it was mine as well.
A few flight and critical care programs require little to no prior training on the ventilator. However, they usually provide formal training. Some programs will give you an 8-hour class and then cut you loose and say good luck, call us if you need anything, and remember that if all else fails, use your BVM. Some programs will even go into greater depth, so you understand the ventilator and how to manage the vent, set you up to shadow an RRT, and even have you do ICU rotations to get you comfortable with the vent.
In this blog, I am going to cover the basics of the ventilator. This is just a quick overview, so stay tuned for more. Let’s break it down so you understand what you are seeing and what the sending facility’s RRT is saying when you walk into a patient’s room.
So, let us start this off with a scenario.
You are dispatched for an IFT from a rural hospital’s ED going to a larger community hospital ICU. You and your partner arrive at the bedside with an RRT relating, “The patient came into the ED for respiratory distress by EMS. We found bilateral infiltrates on the X-ray, and shortly after placing the patient on BiPAP, the patient went into cardiac arrest in the ED. The patient was intubated with an 8.0 endotracheal tube and is secured at 24 at the teeth.
The patient was placed onto “crash” ventilator settings. The patient is 5’8″ with an ideal body weight of 68kg. He is currently on SIMV, Rate of 12, TV of 500, PEEP- 10, PS of 5cmH2o, FiO2 1.0. Plateau pressure of 23-24 and a driving pressure around 13-14. I haven’t been able to draw a blood gas yet, but if you need anything else, let me know, I am the only RRT in the hospital, so I have to go give a breathing treatment. The nurse knows how to reach me.”
Now when reading this scenario, are you confused? Does this seem like a lot of information to take in? My goal for this blog is that when you re-read that scenario, you understand the patient’s mode and understand what other underlying conditions may be present with the patient via the ventilator. As critical care transport providers, we know that mechanical ventilation is complicated, but it doesn’t have to be.
Volume or Pressure?
When it comes to ventilators, you will see several different modes to ventilate a patient. The important thing to remember is that the vent will only work off of two different ways to deliver a breath. These two different ways are Volume or Pressure. Once you select volume or pressure, you will see several other modes of ventilation you can utilize. It is essential to understand what volume does and what pressure does. Once you understand the difference between the two, using a vent will become a lot easier.
So, let us talk about volume mode. You are most likely to see a volume mode used when picking up a patient. Volume-controlled modes work by delivering the preset tidal volume during the inhalation phase of ventilation. When using a volume setting, you will see a constant tidal volume being delivered. When using a volume-controlled mode, it is important to understand that the airway pressures will always vary based on the patient’s respiratory effort and lung compliance. One major disadvantage in this mode is that high airway pressures may be generated and potentially cause barotrauma to your patient. Most ventilators have a cut-off to prevent this barotrauma from happening however, it is still something to pay attention to.
Now that we have discussed volume let us discuss pressure modes of ventilation. When it comes to pressure modes of ventilation, we must understand that, unlike Volume Controlled modes, Pressure controlled modes delivers a breath at a set peak inspiratory pressure (PIP).
When using a pressure-controlled mode on a vent, you are going to set a peak inflation pressure and a respiratory rate. With pressure modes, we are setting up a pressure we want to achieve, not a set tidal volume. You will see varying tidal volumes in your patients based on the patient’s pulmonary status on each respiration. One important thing to pay attention to due to the varying tidal volumes is your patient’s minute ventilation.
For a pressure-controlled mode to be utilized to its fullest potential, you must understand your vent and your patient’s current pulmonary status. For example, if you place an intubated patient who came to the ER with COPD onto a pressure control mode, you may see larger tidal volumes because the patient’s lungs are very compliant. If you have an ARDS patient who was intubated and placed onto a pressure mode, you will notice that the patient will be receiving small tidal volumes due to the patient’s lungs not being as compliant.
The best way to understand the difference between the two is this. If you must directly change the volume on the patient, you are dealing with a volume mode. If you must directly change your patient’s pressures, you are dealing with a pressure mode. You will also see that when working with a patient on a pressure mode, you will see that the volume adjustment is usually blacked out because you cannot change it.
Different modes of Ventilation
Some common modes of ventilatory support you may see are:
- Continuous Mandatory Ventilation (CMV)
- Assist-Control Ventilation (AC)
- Synchronized Intermittent Mandatory Ventilation (SIMV)
- Pressure Support Ventilation (PSV)
- Non-invasive Ventilation (NIV)
Just a slight disclaimer before we dive into these modes of ventilation. When it comes to discussing a volume-controlled breath delivery type, you will see “tidal volumes” being used, but when we discuss pressure-controlled ventilation, we can substitute the wording “tidal volume” for “inspiratory pressure.”
Continuous Mandatory Ventilation (CMV):
This mode works by having the ventilations delivered at a preset rate that you have established on the vent regardless of the patient’s effort. You will see this mode used often when dealing with a paralyzed or apneic patient because it can lead to severe ventilator dyssynchrony if respiratory effort is present. For example, if you set the ventilation rate for 12 on the vent, the patient will receive only those 12 breaths regardless of the patient’s respiratory effort. Dyssynchrony occurs when there is a mismatch between the timing and delivery of mechanical breaths and the patient’s breathing or the patient triggering a breath.
Assist-Control Ventilation (AC):
This mode works by delivering ventilations with the assistance of the patient’s respiratory effort. When the patient triggers a breath, the ventilator essentiality will assist the patient’s breath in achieving the preset tidal volume if allowed. One thing to understand with this mode of ventilation is that you can also preset a respiratory rate. When dealing with AC in a pressure mode, you will notice that you cannot preset the tidal volume, but you will be able to inspiratory time. This will be discussed later. This means that the ventilator will deliver the preset number of ventilations pre-determined by the clinician while allowing the patient to breathe over the pre-determined respiratory rate.
This mode is commonly used on patients who are less sedated. For this reason, it allows for the patient to initiate their own breaths.
Something to be mindful of is that this ventilation mode allows the patient to initiate their own breath. Since they can trigger their own breath, they can run the risk of being over ventilated because when they trigger their own breath, the vent will deliver an assisted ventilation to the preset tidal volume you have determined.
Synchronized Intermittent Mandatory Ventilation (SIMV):
This mode works by delivering preset breaths in coordination with the patient’s respiratory effort. SIMV does allow for spontaneous breaths between ventilations. When setting up the ventilator for this mode, you will set up a respiratory rate along with tidal volume. One thing that makes this mode of ventilation different from assist control is that when the patient delivers a spontaneous breath, they will only achieve the tidal volume they put out. The ventilator will not assist them to a higher preset tidal volume unless additional pressure support is added.
For example: If the tidal volume is set at 500 when the ventilator gives a breath, the patient will achieve a tidal volume of 500. If the patient initiates a breath and the patient is only achieving a tidal volume of 250, that is all they would achieve since it was not a ventilator-triggered breath.
With the same example as above, if the tidal volume is set at 500 when the ventilator gives a breath, the patient will achieve a tidal volume of 500.
If the patient initiates a breath and the patient is only achieving a tidal volume of 250, the additional pressure support added to the ventilator will assist in achieving a tidal volume of 500.
Pressure support ventilation (PSV):
PSV is becoming more popular and is being used more due to studies showing it can limit barotrauma. It is essential that you only use this mode when the patient has spontaneous respirations with an adequate respiratory drive. Patient selection is key in the success of the use of PSV.
This mode differs from the two we previously discussed because this mode is only driven by pressure. This mode works primarily by providing a level of support needed to assist the patient’s spontaneous effort. Essentially the patient determines the tidal volume, respiratory rate, and flow rate.
This mode is primarily used for patients whose respiratory failure is not as severe and have an adequate respiratory drive. When using this mode, be familiar with your ventilator. Some ventilators allow you to set up a backup respiratory rate.
Non-invasive Ventilation (NIV):
There are only two versions you must worry about. These two are Continuous Positive Airway Pressure (CPAP) and Bi-level Positive Pressure Airway Pressure (BiPAP). NIV, over the years, has become the “go-to” treatment in the emergency department for patients who qualify. These modes work by delivering ventilation through an appropriately-sized mask secured onto the patient’s face and not an endotracheal tube.
Now please understand that this mask is different from an NRB mask.
You will see this primarily used for patients with acute exacerbation of chronic obstructive pulmonary disease (COPD), asthma, decompensated congestive heart failure (CHF), or pulmonary edema. In the pre-hospital setting, and usually in the 911 setting, you will commonly see CPAP being used, and when transferred into the hospital setting, BiPAP may be applied.
When it comes to CPAP and BiPAP, it is essential to know the difference between the two. CPAP is more geared towards oxygenation vs. BiPAP that can be used for oxygenation and ventilation. You will commonly hear that BiPAP is a form of CPAP. While this is correct, the difference is that BiPAP alternates between high and low positive airway pressures, whereas CPAP keeps a single, constant pressure throughout the respiratory cycle.
When it comes to BiPAP, it is vital to understand that it assists in ventilation by lowering the pressure the patient must exhale against while still offering pressure to stent alveoli open to still allow for gas exchange. BiPAP also helps with ventilation by augmenting tidal volumes with higher IPAP, which can be useful to increase minute volume ventilation and blow off excess CO2.
Let’s talk about Parameters.
Now let us talk about the other portion of the scenario when you saw the words “Plateau Pressure” and “Driving Pressure“. Another one we are also going to cover is Peak Inspiratory Pressure (PIP), dead space, and i:e times.
Plateau pressure:
This is the pressure that is applied to the alveoli and smaller airways during mechanical ventilation. When in a volume-controlled mode, the plateau pressure is measured at the end of the inspiratory pause. When using pressure-controlled ventilation, the plateau pressure is measured at the end of the inspiration phase. You will commonly see the Plateau pressure documented or seen as Pplat. Ideally, we want to see this below 30cmH20. This is showing the measurement of alveolar compliance.
Driving pressure:
The equation for calculating driving pressure is Pplat – PEEP. Ideally, we want this less than 15cmH20 because it shows us the amount of forces being applied to the alveoli. It has been expressed that this is the ratio of the tidal volume to the compliance of the respiratory system. If you encounter a larger force being used, you can potentially correct the issue by adding PEEP.
Peak Inspiratory Pressure (PIP):
PIP is measured during the inhalation phase. It is the highest level of pressure applied to the lungs during that phase. Ideally, we want this number to be lower than 35 cmH20.
Dead space:
Dead space is the volume of air that is inhaled but does not take part in the gas exchange. Now when you dive deeper into vent management, you will discover two forms of dead space. One being anatomic dead space and the other being alveolar dead space.
Anatomic dead space is the volume of air that is in the respiratory tract that is not involved in the gas exchange. Alveolar dead space is the volume of air that is being ventilated and not perfused. Since it is not being perfused, gas exchange does not take place.
Understanding I:E
When it comes to I:E times, it is important to understand the meanings. (i) stands for inspiratory time, and (e) stands for expiratory time.
In a normal adult who spontaneously breathes, the expiratory time is about twice as long as the inspiratory time. You will commonly see I:E times of 1:2. (i) is one second: (e) is two seconds. In a normal pediatric patient, the standard i:e is 1:3, and in infants, it is 1:4.
It is important to understand that clinicians will tend to see lengthy expiratory phases in patients who have obstructive pathologies.
Listen to your Alarms!!! Here is why!
Now please listen for the vent alarms!! 99% of the time, it is the vent telling you something. Do not just hit the silent button and move on.
When it comes to the vent alarms, here are some of the most common alarms and the reasons why. One thing to understand though is that the LTV and Revel vents tend to stack alarms, so please scroll through them.
Also, do not forget about DOPE! It is important that we do not get tunnel-visioned into thinking that it’s the vent having an issue.
D: Displacement of Endotracheal tube.
O: Obstruction of the endotracheal tube.
P: Pneumothorax.
E: Equipment failure.
Most Common Alarms you may see and why you may see them:
High Pressure (Aka obstructive):
- Secretions in ETT/Airway.
- Kink in Vent tubing
- Patient biting on ETT
- Patient coughing, gagging, or trying to talk.
- Increased airway pressure or pneumothorax.
Low Pressure (Aka disconnect):
- Vent tubing is not connected.
- Vent tubing leak.
- Displaced ETT/Trach tube.
- Ruptured cuff at the end of the endotracheal tube.
When it comes to ventilators, there are several out there that you are going to see at the hospitals. Nevertheless, I want you to see the four most common transport ventilators you may be working with.
If you have any other questions regarding vents, please feel free to sign up for our Flight Medical Provider Course or check out more on the subject of ventilators from the perspective of a nurse!
- References:
- Andres L. Mora Carpio; Jorge I. Mora. Assist Control. April 2021. https://www.ncbi.nlm.nih.gov/books/NBK441856/
- Allon Amitai, MD. Ventilator management. April 2020.Ventilator Management: Introduction to Ventilator Management, Modes of Mechanical Ventilation, Methods of Ventilatory Support
- Christopher D Jackson MD. Mechanical Ventilation. September 2020. Ventilator Management: Introduction to Ventilator Management, Modes of Mechanical Ventilation, Methods of Ventilatory Support
- Chris Smetana, Lindsay Mauldin, Sheila Moak, Mike Boone. Flight Medical Provider: A Ground and Flight Critical Care Guide (IA MED). Gwenny Cavin and Michael Carunchio.
- Alarm meme: https://memegenerator.net/instance/80256832/john-goodman-am-i-the-only-one-here-who-cares-that-the-vent-alarms-are-going-off